The United States is currently balancing on a precarious edge, facing the imminent loss of its historic measles elimination status—a public health designation held since 2000. As of late January 2026, confirmed measles cases have surged past 400 nationwide, driven by active outbreaks in states like South Carolina, Texas, and Arizona. This resurgence coincides with a controversial and sweeping overhaul of the CDC vaccine schedule overhaul announced earlier this month, which has left parents and pediatricians scrambling to interpret new "shared decision-making" guidelines. With federal health policy shifting dramatically under new HHS leadership, the nation faces a perfect storm of policy confusion and rising infection rates.
New CDC Vaccine Schedule Overhaul Creates Widespread Confusion
On January 5, 2026, the Department of Health and Human Services (HHS) finalized a major restructuring of the childhood immunization schedule. In a move described by officials as an effort to align with "peer nations," the CDC has reclassified several vaccines that were previously recommended for all children. This profound shift has introduced a new category of immunizations based on "shared clinical decision-making," fundamentally changing how pediatric care is delivered in the United States.
Under the new childhood immunization requirements 2026 framework, vaccines for influenza, COVID-19, rotavirus, hepatitis A, hepatitis B, and meningococcal disease are no longer universally recommended for healthy children by default. Instead, these shots are now subject to individual discussions between parents and providers. Only ten "consensus" vaccines—including Measles, Mumps, Rubella (MMR), Polio, and Tetanus—remain on the routine schedule for all children. This abrupt policy change has sparked intense debate and confusion regarding insurance coverage and state-level school entry mandates.
What "Shared Decision-Making" Means for Parents
The transition to a vaccine shared decision making model places a heavier burden on parents to evaluate medical risks and benefits. While HHS officials argue this approach reduces "coercion" and respects parental autonomy, pediatric groups warn it may lead to dangerous gaps in immunity. For many families, the immediate practical question is whether these non-routine vaccines are still required for school enrollment. Since school mandates are determined by state laws—many of which reference CDC guidelines—local school districts are currently struggling to provide clear answers to anxious parents.
Measles Elimination Status US: A Designation at Risk
The measles elimination status US is now under formal review. Elimination is defined as the absence of continuous disease transmission for 12 months or more in a specific geographic area. Epidemiology reports indicate that the U.S. has likely breached this threshold due to a chain of transmission that began in late 2025 and has continued uninterrupted into January 2026. The Pan American Health Organization (PAHO) is scheduled to meet in April to review the data, but many experts believe the decision is already a foregone conclusion.
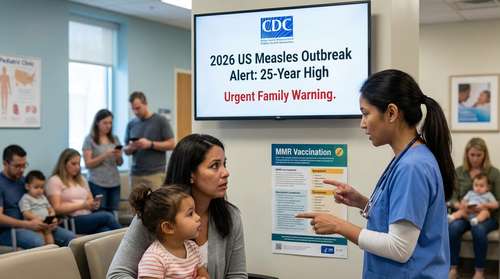
Public health officials have identified active transmission chains in over 14 jurisdictions. The speed of the spread is alarming; while the U.S. recorded roughly 2,200 cases throughout all of 2025, the first three weeks of 2026 alone have seen over 400 confirmed cases. This acceleration suggests that herd immunity thresholds—typically requiring 95% vaccination coverage—are fraying in key communities. If the U.S. loses its elimination status, it would join a small list of nations that have seen a resurgence of the virus after successfully eradicating it.
Pediatric Health Alerts for Parents: Navigating the Outbreak
In response to the rising case numbers, medical associations have issued urgent pediatric health alerts for parents. The most critical advice remains unchanged: the MMR vaccine is highly effective and remains on the "routine" list under the new CDC guidance. Pediatricians are urging parents to check their children's vaccination records immediately, especially if they reside in outbreak hotspots like the Midwest or the Sun Belt.
Symptoms of measles often begin with a high fever, cough, runny nose, and red, watery eyes, followed days later by a characteristic rash. The virus is incredibly contagious; it can linger in the air for up to two hours after an infected person leaves a room. With the 2026 measles outbreak news dominating headlines, doctors emphasize that vaccination is the only reliable shield against severe complications, which can include pneumonia and encephalitis.
HHS Health Policy Updates and Future Implications
The recent HHS health policy updates represent more than just a schedule change; they signal a philosophical pivot in American public health strategy. By narrowing the list of universally recommended vaccines, federal authorities are betting that a more targeted approach will rebuild trust. However, critics argue that de-emphasizing vaccines like Hepatitis B and meningitis shots could lead to a resurgence of diseases that have been suppressed for decades.
As schools and insurance companies react to these federal changes, parents should expect a volatile few months. While the Affordable Care Act (ACA) provisions generally require coverage for CDC-recommended vaccines, the new "shared decision-making" classification adds a layer of complexity to billing and coverage determinations. Families are advised to consult directly with their insurance providers and local school boards to understand their specific obligations and coverage rights in this shifting landscape.