In a historic and controversial shift that effectively rewrites the playbook for American pediatric health, the Centers for Disease Control and Prevention (CDC) has released its CDC vaccine schedule 2026, slashing the number of universally recommended childhood immunizations from 17 to 11. The overhaul, announced officially on January 5 and spearheaded by the Department of Health and Human Services (HHS), moves common vaccines—including those for Influenza, Hepatitis A and B, and COVID-19—from a routine status to a new “shared clinical decision-making” model. The move has ignited a firestorm of debate between federal officials and the medical establishment, marking one of the most significant pivots in pediatric health news in decades.
From Routine to ‘Shared Decision-Making’: What Changed?
The core of the new 2026 guidance is the reclassification of nearly a third of the previously standard vaccine roster. Under the new childhood immunization guidelines, the CDC no longer recommends a default “universal” administration for vaccines protecting against Influenza, Rotavirus, Hepatitis A, Hepatitis B, and COVID-19. Instead, these shots now fall under “Shared Clinical Decision-Making” (SCDM). Additionally, immunization against Respiratory Syncytial Virus (RSV) has been moved to a “High-Risk” category, recommended only for specific vulnerable populations.
Practically, this means the default answer at a pediatrician’s office is no longer “yes” for these shots. Instead, providers are instructed to discuss the risks and benefits with parents on a case-by-case basis. The remaining 11 universally recommended vaccines—which include measles, mumps, rubella (MMR), polio, and tetanus—remain on the routine schedule, though the HPV regimen has been notably reduced from two doses to one.
The ‘Denmark Model’: Rationale Behind the Shift
The rationale for this drastic reduction, according to HHS officials, is to align the United States with “peer nations” in Europe, specifically citing Denmark’s streamlined immunization schedule. The administration argues that the previous schedule was bloated and that the shift toward shared decision-making vaccines empowers parents and reduces “coercion” in medical care.
“We are aligning the U.S. childhood vaccine schedule with international consensus while strengthening transparency,” officials stated in the January announcement. The goal, they argue, is to rebuild public trust by focusing routine recommendations only on diseases where there is global agreement on the necessity of universal vaccination.
Medical Community and States Push Back
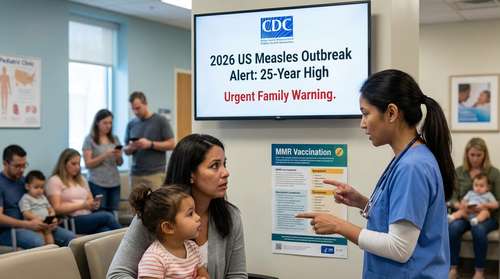
The reaction from the medical community has been swift and fierce. The American Academy of Pediatrics (AAP), along with the American Medical Association (AMA) and other public health groups, have condemned the changes as “dangerous and unnecessary,” warning that removing the universal recommendation for diseases like Hepatitis B and the Flu could lead to a resurgence of preventable illnesses.
As of this week, major medical organizations have filed lawsuits seeking to reverse the decision, calling the overhaul unlawful and lacking in scientific evidentiary support. Furthermore, a growing vaccine policy controversy is playing out at the state level. Health departments in California, New York, Massachusetts, and Minnesota have publicly rejected the new federal guidance, stating they will continue to enforce the previous, more comprehensive immunization standards for their residents.
Impact on School Mandates and Insurance
For parents, the most pressing question is how these changes affect mandatory vaccines for school. While the CDC sets guidance, individual states determine school entry requirements. With the federal recommendation withdrawn, there is confusion over whether schools in states that defer to CDC guidelines will automatically drop requirements for Hepatitis B or Meningococcal vaccines. Legal experts anticipate a patchwork of regulations emerging across the country throughout 2026.
Despite the rollback in recommendations, HHS has confirmed that all vaccines, including those moved to the SCDM category, will continue to be covered by insurance plans and the Vaccines for Children program through the end of the year. However, doctors fear that without the “routine” label, long-term access and insurance coverage could eventually erode, exacerbating family health trends 2026 toward lower immunization rates.