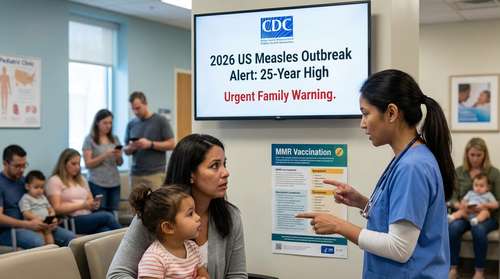
February 15, 2026 – In a seismic shift that has left pediatricians scrambling and millions of parents re-evaluating their healthcare plans, the Centers for Disease Control and Prevention (CDC) and Department of Health and Human Services (HHS) have officially implemented a slashed 2026 CDC vaccine schedule. The landmark revision reduces the number of universally recommended childhood immunizations from 17 down to just 11 core childhood vaccines, moving major shots like Hepatitis B, Influenza, and RSV into a new optional category. As families navigate these sudden childhood immunization updates, the standard well-child visit is undergoing its most significant transformation in decades.
The New "11 Core" Model: What Changed?
Under the directive of HHS Secretary Robert F. Kennedy Jr. and Acting CDC Director Jim O'Neill, the federal government has pivoted to a "consensus-based" model aligned with nations like Denmark and Japan. The new pediatric health guidelines 2026 prioritize a streamlined list of protections deemed essential for all children, while categorizing others as discretionary.
The 11 core childhood vaccines that remain universally recommended include:
- Measles, Mumps, and Rubella (MMR)
- Diphtheria, Tetanus, and Pertussis (DTaP)
- Polio (IPV)
- Haemophilus influenzae type b (Hib)
- Pneumococcal disease
- Varicella (Chickenpox)
- Human Papillomavirus (HPV) – Revised to a single-dose regimen
Notably absent from the mandatory roster are vaccines for Hepatitis A, Hepatitis B, Influenza (Flu), COVID-19, Rotavirus, and Meningococcal disease. These have not been banned but have been reclassified under a new protocol known as shared clinical decision-making.
Understanding "Shared Clinical Decision-Making"
For decades, the default stance of the American medical establishment was simple: if a vaccine is on the schedule, every child gets it. The shared clinical decision-making vaccines model upends this default. Doctors are now instructed to discuss these specific immunizations with parents on a case-by-case basis, weighing individual risk factors, local outbreak data, and family preference.
"This approach eliminates the 'one-size-fits-all' mandate," Secretary Kennedy stated in the press briefing. "It empowers parents to make informed choices with their providers without the pressure of a universal recommendation."
However, this shift puts immense pressure on well-child visit changes. Pediatricians warn that 15-minute appointments are no longer sufficient to cover the complex risk-benefit discussions required for six or seven optional vaccines. "We are effectively asking parents to become amateur epidemiologists," says Dr. Elena Rodriguez, a pediatrician in Ohio. "The burden of decision is shifting from public health policy to the exam room."
Well-Child Visits: A New Era of Negotiation
As family health news 2026 dominates headlines, the practical reality is hitting clinics this week. Parents attending routine check-ups are finding themselves in lengthy negotiations. The removal of the Hepatitis B birth dose—previously a standard safeguard against liver disease given within 24 hours of life—has been particularly contentious, with many hospitals now requiring explicit parental requests to administer it.
Furthermore, the RSV immunization, previously rolled out to protect infants from severe respiratory distress, is now strictly categorized for "high-risk" populations only. This leaves millions of healthy infants without a default recommendation for RSV protection, a move that critics argue could lead to a surge in winter hospitalizations.
Does Insurance Still Cover the Optional Shots?
One of the biggest sources of confusion involves cost. Despite the downgrade from "universal" to "shared decision," HHS has confirmed that all vaccines on the previous schedule will remain fully covered by insurance plans, Medicaid, and the Vaccines for Children (VFC) program. The Affordable Care Act mandates coverage for ACIP-listed vaccines, and the new "shared decision" category preserves this listing status, ensuring that families who choose to vaccinate against Flu or Hep B will not face out-of-pocket costs.
The "Denmark Model" Controversy
The administration cites the "Denmark Model" as the blueprint for these pediatric health guidelines 2026, noting that Scandinavian nations often have shorter schedules and healthy populations. Proponents argue this will reduce vaccine hesitancy by focusing on the most critical diseases. "By recommending fewer shots, we hope to restore trust in the ones that matter most, like measles and polio," stated Acting Director O'Neill.
Public health experts, however, are sounding the alarm. They contend that the U.S. has a different demographic and healthcare landscape than Denmark, and stripping away herd immunity protections for diseases like Rotavirus and Influenza could trigger avoidable outbreaks. As families navigate this brave new world of pediatric care, the advice from most medical associations remains steady: consult your doctor, ask questions, and ensure your child is protected against the full range of preventable diseases, regardless of the new federal classification.