February 9, 2026 – The landscape of childhood health took a dramatic turn this week as the U.S. Centers for Disease Control and Prevention (CDC) solidified its 2026 immunization guidance, officially reducing the number of universally recommended childhood vaccines from 17 to 11. This unprecedented shift, which aims to align U.S. policy with international standards like those in Denmark, has sparked confusion among parents and a sharp divide between federal agencies and private pediatric organizations.
For parents navigating these childhood immunization updates, the changes are significant. The new schedule introduces a tiered approach, moving several previously routine shots—including those for influenza, hepatitis B, and COVID-19—into a category known as "Shared Clinical Decision-Making." As of today, families are facing a confusing reality: an official CDC schedule that contradicts the advice of the American Academy of Pediatrics (AAP), leaving many to wonder which path to follow for their children's health.
The New Core 11: Which Vaccines Remain Universally Recommended?
Under the revised 2026 CDC vaccine schedule, the list of immunizations recommended for all healthy children has been trimmed to focus on diseases deemed the most severe and highly transmissible. Federal health officials emphasize that this "core list" maintains protection against historic scourges while reducing the total injection burden on infants.
The 11 vaccines that remain universally recommended include:
- Measles, Mumps, and Rubella (MMR): Remains a cornerstone of the schedule.
- Polio (IPV): No changes to the dosing schedule.
- Diphtheria, Tetanus, and Pertussis (DTaP): Continue to be routine.
- Varicella (Chickenpox): Remains universally recommended.
- Haemophilus influenzae type b (Hib): Critical for preventing bacterial meningitis.
- Pneumococcal disease: Routine recommendation stands.
- Human Papillomavirus (HPV): Notable Change: The CDC now recommends a single dose rather than the previously standard two-dose series, citing recent efficiency data.
These core shots are still expected to be required for school entry in most states, although state-level legislation is currently in flux following the federal announcement.
Understanding "Shared Clinical Decision-Making"
The most controversial aspect of the pediatric vaccine changes is the reclassification of several major vaccines. Shots that were once automatic checkboxes at a well-child visit are now subject to vaccine shared decision making. This means they are not routinely recommended for every child but should be given based on a conversation between the parent and the doctor regarding specific risks.
Vaccines moved to this category include:
- Influenza (Flu): No longer routine for all; recommended based on individual risk.
- Hepatitis B: The birth dose is no longer universal; it is now a discussion point for parents and providers.
- Hepatitis A: Moved to shared decision-making.
- Rotavirus: No longer universally routine.
- COVID-19: Remains available but not universally urged for healthy children.
- Meningococcal disease: Now targeted primarily at high-risk groups.
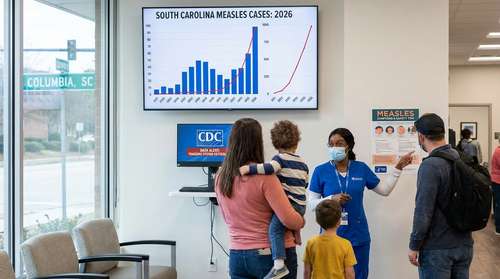
Health and Human Services (HHS) officials argue this shift empowers parents and reduces "vaccine fatigue." However, critics worry that removing the "routine" label will lead to precipitous drops in coverage, potentially sparking outbreaks of diseases like the flu or hepatitis in communities with low immunity.
The Clash: AAP vs. CDC Guidelines
As of February 9, 2026, a unique situation has emerged: the United States effectively has two opposing childhood vaccine schedules. While the CDC has trimmed the list, the American Academy of Pediatrics (AAP) has reaffirmed its commitment to the previous comprehensive schedule, advising pediatricians to continue recommending all 17 vaccines.
This divergence places pediatricians in a difficult position. Many hospital systems and private practices have announced they will adhere to the AAP guidelines, citing the extensive evidence base for shots like the Hepatitis B birth dose. For parents, this means your pediatrician might recommend shots that the CDC no longer explicitly lists as "routine," requiring active participation in medical decisions.
Will Insurance Still Cover Non-Routine Vaccines?
A primary concern for families is health insurance child vaccines coverage. The Affordable Care Act (ACA) mandates coverage for vaccines recommended by the Advisory Committee on Immunization Practices (ACIP). Despite the changes, HHS has confirmed that insurance plans must continue to cover all vaccines that were on the recommended list as of December 31, 2025, for at least the next year.
This means parents who choose to follow the AAP's broader schedule—opting for the flu shot or rotavirus vaccine—should still be able to do so without out-of-pocket costs. However, the long-term coverage landscape for 2027 and beyond remains uncertain if these vaccines remain off the "routine" list permanently.
Navigating the Changes: Advice for Parents
With parenting health news 2026 dominated by these updates, it is easy to feel overwhelmed. Experts suggest a few practical steps:
First, schedule a dedicated appointment to discuss the CDC 11 vaccines list versus the AAP recommendations with your child's doctor. Ask specifically about the risks of skipping the vaccines moved to "shared decision-making" in your local area. Second, check your state's specific school requirements, as state laws often lag behind federal guidance and may still mandate vaccines the CDC has de-emphasized. Finally, rely on trusted medical sources rather than social media when weighing the benefits of vaccines like the annual flu shot.