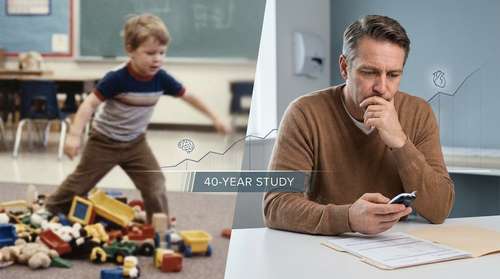
A groundbreaking longitudinal analysis has uncovered a significant connection between childhood ADHD traits and the development of chronic physical health issues nearly four decades later. Published this week in JAMA Network Open, the massive study followed nearly 11,000 individuals from childhood into their mid-40s, providing some of the most robust evidence to date regarding the childhood ADHD long-term effects on systemic health. The findings suggest that the impact of neurodivergence extends far beyond the classroom, influencing cardiovascular, metabolic, and neurological health well into middle age.
The 1970 British Cohort Study: Tracking Health Across a Lifetime
The research, led by a collaborative team from University College London (UCL) and the University of Liverpool, utilized data from the 1970 British Cohort Study (BCS70). This extensive project has tracked the lives of thousands of people born in Great Britain during a single week in 1970. By analyzing this rich dataset, researchers were able to correlate behavioral assessments made at age 10 with physical health outcomes reported at age 46.
Unlike previous research that often focuses solely on clinically diagnosed individuals, this longitudinal ADHD study 2026 examined ADHD traits—such as impulsivity, inattention, and restlessness—identified by parents and teachers. This distinction is crucial because it captures a broader population, including those who may have never received a formal diagnosis but still lived with the underlying neurodevelopmental characteristics.
Key Findings: The Midlife Health Gap
The results paint a stark picture of the ADHD health risks in adults. Participants who exhibited elevated ADHD traits in childhood were found to be 14% more likely to suffer from multimorbidity—the presence of two or more chronic health conditions—by their mid-40s. Specifically, 42% of the high-trait group reported multiple chronic issues compared to 37% of their peers with fewer traits.
The range of conditions linked to these early traits was extensive, including:
- Migraines and chronic pain conditions
- Back problems
- Metabolic disorders like diabetes
- Epilepsy
- Cardiovascular issues
Connecting the Dots: Why Does Neurodivergence Affect Physical Health?
One of the most valuable aspects of this new research is its exploration of why these associations exist. The study didn't just find a correlation; it identified distinct pathways linking ADHD traits and chronic illness. The researchers discovered that lifestyle factors and co-occurring mental health challenges played a significant mediating role.
Individuals with higher ADHD traits were more statistically likely to smoke, have a higher Body Mass Index (BMI), and experience psychological distress in adulthood. These factors collectively explained a portion of the increased physical health risk. This aligns with broader mental health trends 2026, which increasingly view neurodivergence not as an isolated brain difference, but as a factor that influences lifestyle choices and healthcare access.
Professor Joshua Stott, the study’s senior author from UCL, emphasized that these outcomes are not inevitable but rather the result of systemic gaps. "People with ADHD can thrive with the right support," Stott noted in a press release, "but this is often lacking, both due to a shortage of tailored support services and because ADHD remains underdiagnosed."
Gender Disparities in Health Outcomes
The study also highlighted a critical gender dimension to ADHD midlife health impacts. While both men and women with childhood ADHD traits faced increased risks of physical illness, the functional impact of these illnesses appeared more severe in women.
Women with high childhood ADHD traits were significantly more likely than their male counterparts to report that their physical health resulted in disability—limiting their ability to work or perform daily activities. This finding points to a potential "double burden" for women, who are historically underdiagnosed with ADHD in childhood and may lack appropriate coping mechanisms or medical support until much later in life.
The "Hidden" Risk of Undiagnosed ADHD
Perhaps the most alarming implication of this study concerns the millions of adults currently navigating midlife with undiagnosed neurodivergence health outcomes. Since the study looked at traits rather than just medical records, it suggests that sub-clinical ADHD behaviors—often dismissed as "daydreaming" or "fidgeting" in the 1970s and 80s—can act as silent predictors for future health decline.
The mechanism often involves the brain's dopamine reward system. The difficulty with impulse control inherent in ADHD can make maintaining long-term health behaviors—like consistent exercise, balanced diet, and smoking cessation—significantly more challenging. Without a diagnosis and treatment plan (such as medication or CBT), these individuals may struggle to adhere to the lifestyle changes necessary to prevent chronic disease.
Implications for Future Healthcare
As we move further into 2026, the medical community is being urged to adopt a more holistic view of ADHD. It is no longer sufficient to treat it merely as a disorder of attention or academic performance. This data argues for integrating physical health monitoring into the standard of care for neurodivergent patients.
For adults who suspect they may have had undiagnosed ADHD traits in childhood, this study serves as a prompt to prioritize preventative health screenings. Monitoring blood pressure, blood sugar, and musculoskeletal health is particularly vital. Furthermore, clinicians treating patients for conditions like diabetes or chronic back pain may need to screen for underlying ADHD traits to ensure their treatment plans are realistic and sustainable for the patient's specific neurotype.
Ultimately, this decades-long observation underscores a vital truth: mental and physical health are inextricably linked. By addressing the neurodevelopmental needs of children today, we are likely investing in the prevention of chronic physical disease forty years down the line.