Pandemic triggers 25% increase in global prevalence of anxiety, depression
By
Josh Piers

The COVID-19 pandemic has resulted in a 25% increase in the prevalence of anxiety and sadness over the world. The World Health Organization is calling on all countries to improve mental health services and assistance.
Understandably, the worldwide impact of a fatal virus became a key priority, and the practical efforts we took to restrict COVID-19's spread and preserve lives were critical. But it wasn't long before it became evident that there would be another health catastrophe — this time a mental health emergency.
Even though the limits have been eased nearly three years after the initial statewide lockdown, we are still suffering the impacts.
Two-thirds of adults with mental health problems feel their illness has worsened since the first nationwide lockdown, according to a poll conducted by mental health charity Mind. During the epidemic, one out of every four adults experienced mental suffering for the first time.
There is now cross-sectional evidence to indicate a link between loneliness and a variety of mental diseases, such as anxiety, depression, and psychosis, as well as a link between loneliness and suicidal thoughts and behavior.
According to a recent study, loneliness was closely linked to the onset of dementia, and rates were particularly high among persons who had paranoia or psychotic symptoms.
It also discovered that loneliness was linked to suicide attempts and depressed symptoms, however the majority of the studies in the review were cross-sectional and of low quality.
In a systematic analysis of longitudinal studies, people who experienced loneliness were found to have a much higher chance of becoming sad and anxious.
When combined with the fact that loneliness and a lack of social support are predictors of poorer outcomes in people with depression, these findings suggest that anti-loneliness therapies should have an influence on depression and social anxiety as well.
A quick systematic review looked into the influence of loneliness on the mental health of previously healthy children and adolescents.
Although that evaluation will need to be updated when more information about COVID-19 becomes available, the review found research that suggested social isolation and loneliness increased the risk of depression and potentially anxiety at the time loneliness was measured and for the next 0.25 to 9 years.
As a result, the data imply that loneliness has both short and long-term effects on depression.
Multiple stress factors
One key reason for the surge is the tremendous stress brought on by the pandemic's social isolation. Constraints on people's capacity to work, seek support from loved ones, and participate in their communities were all linked to this.
Loneliness, fear of infection, pain and death for oneself and loved ones, sadness following a bereavement, and financial problems have all been identified as stressors that contribute to anxiety and depression. Exhaustion has been identified as a primary factor for suicide trigger among health care professionals.
People who were more likely to have mental health issues prior to the pandemic have felt the brunt of the effects. They're reporting an increase in the severity of current issues, as well as fears about the future. They require immediate assistance.
Young people and women are the hardest hit.
The brief, which is based on a comprehensive review of existing evidence about COVID-19's impact on mental health and mental health services and includes estimates from the most recent Global Burden of Disease study, shows that the pandemic has harmed young people's mental health and that they are disproportionately at risk of suicidal and self-harming behavior. It also suggests that women have been hit harder than males, and that persons with pre-existing physical health illnesses like asthma, cancer, or heart disease are more likely to experience mental health symptoms.
People with pre-existing mental illnesses do not appear to be disproportionately sensitive to COVID-19 infection, according to the data.
Gaps in health care
This rise in mental health problems has coincided with substantial interruptions in mental health services, creating large gaps in care for people who need it the most. Among all basic health care, services for mental, neurological, and drug use disorders were the most affected for much of the pandemic. People receiving benefits have been hit particularly hard and are experiencing increasingly severe and complex problems.
What's Your Reaction?
Share this article
Author
Related Posts
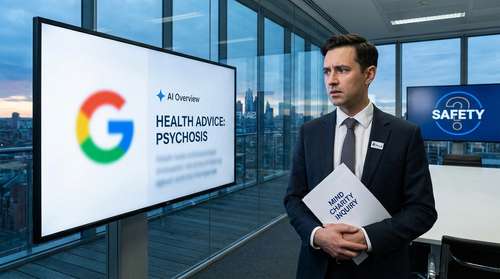
Mind Launches Major Inquiry into AI Safety After 'Very Dangerous' Mental Health Advice Exposed

The 'Hidden' Anxiety: New APA Study Links Food Insecurity to Rising US Workplace Mental Health Crisis

Zuckerberg Testifies in Historic Teen Mental Health Trial: "I Wish We Got There Sooner"
